By Julia Finlay.
Until quite recently, medical advice for low back pain was rest and painkillers. But clinical trials have shown that keeping moving, even if it’s painful, creates much better outcomes for back pain sufferers. Why would that be?
Well to begin with, bed rest weakens us really quickly. Studies show a 12% decline in muscle strength per week (1) and commensurate loss of muscle mass . Which means that if we stop moving, it makes it even harder to get going again. And weakening tummy muscles in particular will mean that we have even less support for our back than we previously had before the back pain kicked in. We need integrated muscle movement that manages the whole spine in the context of the whole body. (See also below)
Recent studies show that back pain is typically, like much of life, multifactorial. When we take case histories as osteopaths, we always ask about current stressors in life, as this is typically in the picture of many acute episodes. It can be frightening to move if you are in acute pain, as the internal signalling is designed to make us take care. But perhaps best to view pain as a guide to careful movement, not an excuse not to try. Fear of movement is after all quite a negative choice; we might all prefer to keep moving forward in life rather than stand still- both literally and metaphorically!
Beyond this, our attitudes to pain and understanding of it, the “meaning” it has for us (if you like) also have a bearing. As do a multitude of other factors including diet, exercise, smoking, alcohol … in fact here’s a diagram that pulls current understanding together
Contributing factors for Back Pain
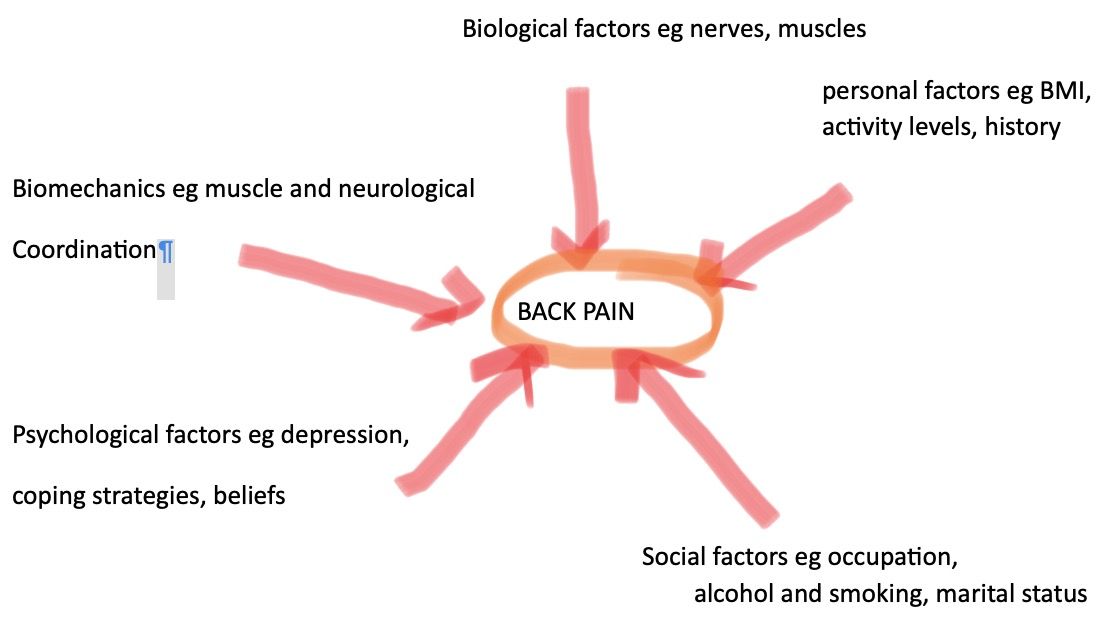
After Source (4)
Additionally, bone health and density is linked to use, and weight-bearing exercise. Walking counts here. Every step we take stimulates the cells in our bones to keep metabolising bone to keep us strong and keep the calcium in our bones. When we rest our cells also respond – by taking calcium out of bone to use for other things, which can ultimately predispose us to kidney stones. This applies to all bones in the body, not just legs, pelvis and lower back. They all need movement to stimulate bone health and strength. So resting weakens bone, and also impacts our sense of wellbeing, lung and heart health, immune system function, and more besides.
But rather than dwell on the downsides of rest, perhaps we should think about the benefits of movement? During our osteopathic training we were shown time and again that movement and health are almost equivalent for our bodies, both as a whole and in part. NICE guidelines (2) now minimise use of “RICE” (Rest, Ice, Compression, Elevation) for ankle sprains because again it has been shown that tissues repair better when they are moved – it helps strength and blood flow which brings healing faster.
Finally, all movement and exercise help the body as a whole. All our joints are supported by all our bones, muscles and other joints. You can think of the body as being held together by inner elastic (fascia) which is always in reciprocal tension so that as one bit of us moves, all of our body adjusts to the movement. This is a principle known as Tensegrity (3), and it helps us counteract gravity. So the joints in our lower backs need the joints in our pelvis and shoulders to be working well to help them stay healthy and not get compressed by our own weight . Exercise like pilates and yoga help the whole system function well together, and reinforce healthy movement patterns. But as far as exercise goes, often the best is the type you most enjoy and can access most easily.
So even if you are feeling a bit crocked, try and keep going, you’ll feel better for it and recover more quickly. Let us know if you need a bit of help to speed your recovery!
2. https://cks.nice.org.uk/sprains-and-strains#!scenario
3. https://www.anatomytrains.com/fascia/tensegrity/
4. Farrokhi, Shawn, Brittney Mazzone, Michael Schneider, Sara Gombatto, John Mayer, M. Jason Highsmith, and Brad D. Hendershot. “Biopsychosocial risk factors associated with chronic low back pain after lower limb amputation.” Medical hypotheses108 (2017): 1-9




